7 Misconceptions about Insurance Fraud Investigations
Crime Statistics
Fraud offences can take many forms and have become more common as technology becomes more accessible. They can result in victims and Canadian businesses losing significant amounts of money or property according to a 2021 report from the Canadian Anti-Fraud Centre. Statistics Canada provides annual financial crime data on fraud trends across the country, as a general rule, fraud charges are less common than theft.
Our Experience
Insurance fraud investigations can be difficult to navigate, especially for someone who is inexperienced. This, in many cases, leads to mistakes along that way that can be very costly. The best way to protect your rights if you have been accused of insurance benefit fraud is to hire experienced legal counsel to negotiate on your behalf.
An individual may become involved in an insurance investigation in a few different ways. One of the most common ways insurance providers begin investigating someone is through random audits. All large employment insurance benefit providers like Sunlife Financial and Manulife Financial conduct random audits on employees using their benefits. During these audits, benefit providers will review employee benefit files to ensure they received only the funds they were entitled to. They may also verify receipts provided by contacting the service provider to confirm the client received services there as indicated in their claim. The Firm has been involved in many insurance fraud investigations which are often are investigated and prosecuted by local police, which are referred by employers and insurance companies. Regulated professionals such as Teachers, Accountants, Nurses and Financial Service workers are all being aggressively investigated and being reported in caselaw.
In other situations, plan benefit holders may be audited if they have received services from a service provider that has been delisted. Insurance companies will delist any service provider who fails to abide by the terms and conditions of the benefit plan. They will also delist service providers who commit fraud. After delisting a service provider, the insurance company may then audit any individuals who claimed benefits from that particular service provider. This strategy has become more popular in recent years after sophisticated employee benefit fraud schemes

- Lexpert: How companies can protect themselves against internal thefts.
- Global News Morning Show: Sentencing Arguments in Assault case of Dafonte Miller.
- Breakfast Television: Role of Mental Health in Court Proceedings.
- Global News National: Bruce McArthur will not serve consecutive sentences.
- CBC Radio: Interview with Mayor John Tory and Jordan Donich on CBC Radio.
- CTV News National: Handgun ban supported by majority of Canadians: Nanos survey.
- Global News: How difficult is it to get a legal handgun in Canada.
- CP24: Sentencing Hearing for Chair Girl.


In 2014, the TTC received a tip that its employees were defrauding Manulife Financial out of employee benefits. During the investigation it was discovered that hundreds of TTC employees had been receiving false or inflated receipts for services from a provider called Healthy Fit. The employees submitted the false claims to Manulife and then paid a kickback to Healthy Fit. This sophisticated scheme resulted in thousands of dollars in losses for Manulife. Ten employees and the proprietor of Healthy Fit were ultimately charged criminally with fraud and over 200 other employees were terminated or resigned from their positions at the TTC. Regardless of how an investigation begins, once an insurance company has launched a joint investigation with a plan member’s employer, it is almost impossible to stop and can result in serious consequences for those who are found to have abused their benefits plan.
The Firm has represented plan members from across Canada including British Columbia, Alberta and Newfoundland. Investigations often start in Ontario where the headquarters of large insurance companies are located. In the Firm’s File No. 34****2 it recently represented a nurse in Toronto alleged to have committed $3500 in false physiotherapy, massage, naturopath and other related claims in September 2023. The plan member did not have receipts for the claims and was under audit. The Firm was able to resolve the matter secretly without her being terminated, charged or reported to the College of Nurses.
The Firm has also represented several plan members who have resigned, only to have insurance companies, their employer and law enforcement contact them later. In the Firm’s File No. 23****1, it defended the accused alleged to have defrauded $2500 in false benefits claims when she was contacted by investigators months after resigning from her employment in May, 2023. The matter was swiftly resolved prior to reporting to law enforcement in Durham Region. In the Firm’s File No. 64****2 it defended another employee who resigned 6 months prior, he was contacted by Durham Region Police when he retained the Firm. We were able to raise evidentiary problems with the prosecution and negotiated a resolution with the Officer in Charge to avoid charges, fingerprints and photos. This is an aggressive and risky strategy because it can involve the defence providing evidence which could be used against the accused.
The Firm was able to do the same in Airdrie, Alberta with local RCMP in August, 2022 where the the investigating officer wanted to meet both husband and wife in an alleged benefits fraud investigation. The officer was going to lay charges after they resigned months prior in an attempt to flee. The Firm was able to quickly halt the investigation with defence evidence, changing the officer’s grounds for arrest and saving the clients from being charged in its File No. 99****2.
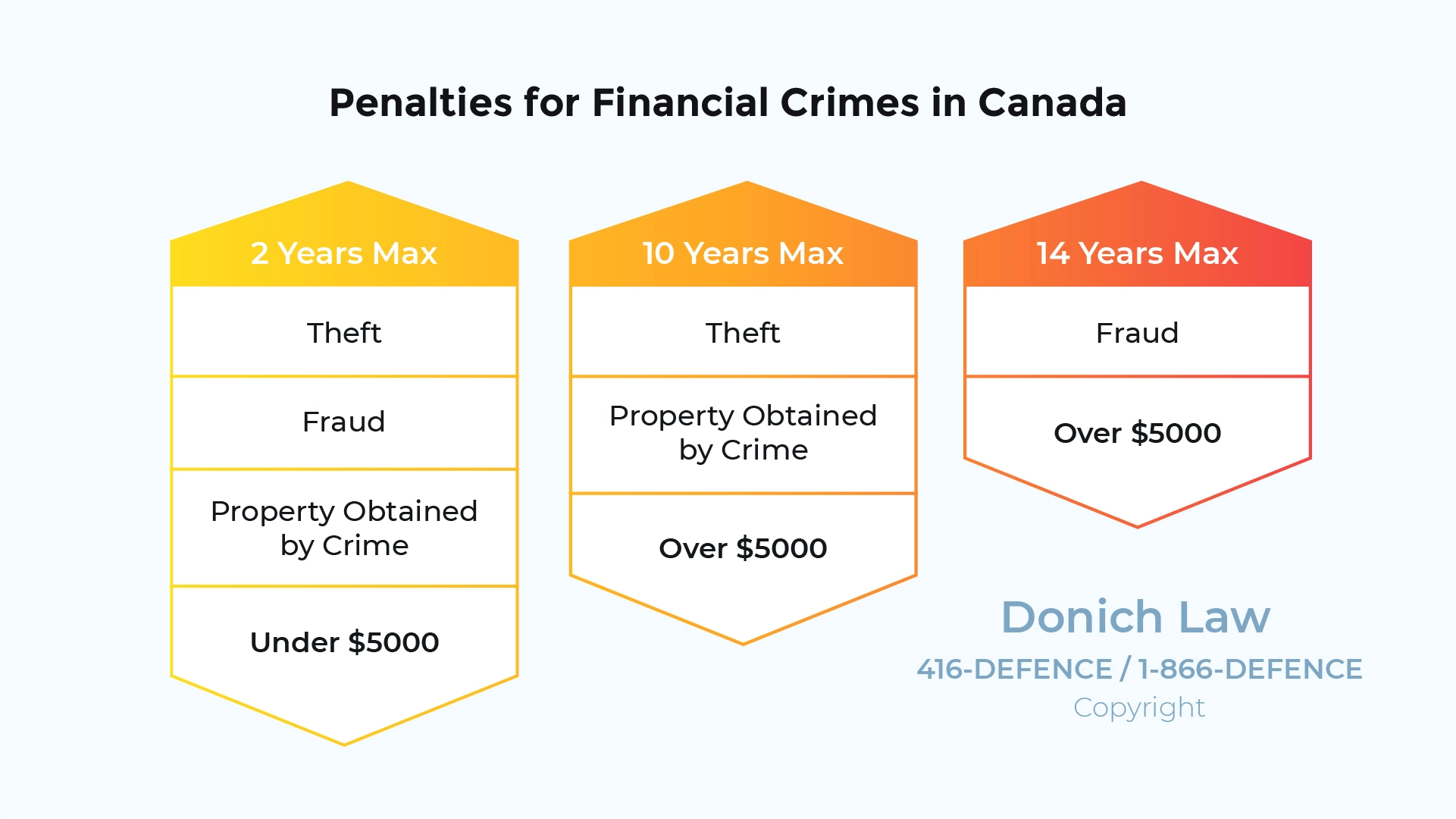
Punishments for Fraud Depend on the Value of the Property
1. Assuming You Will be Forgiven by Apologizing
One of the most common mistakes people make when dealing with an insurance benefit fraud investigation is immediately admitting to everything. Many people have the misconception that if they are honest and tell the truth, they will be given leniency. Others think that because they were a good employee, were well respected or had been with the company for a long time, they will be given a second chance.
This is almost never the case. When dealing with insurance benefit fraud investigations, even the most trusted, well respected, long time employee may face termination, criminal charges or be sued in civil court by their employer or the insurance company.
In many cases, especially in larger companies, reporting policies and shareholder duties are triggered once an employee admits to engaging in fraud related to their employee benefits. In companies with shareholders, there is often a duty that must be discharged, which in many cases may mean pressing charges against an employee who commits fraud.
In many cases, immediately admitting to the fraud and apologizing will do more harm than good for the benefit holder. Firstly, it is unlikely that the apology will hold any weight at all. Just as you cannot apologize your way out of criminal court, you cannot apologize your way out of defrauding your employer or insurance benefit plan provider. Secondly, once you have admitted and apologized for the alleged fraud, it is very easy for your employer or the insurance company to have you charged and convicted and/or sue you in civil court. Finally, if the fraud is reported to law enforcement and charges are laid, the Crown attorney may use any admissions to the employer or insurance company as evidence in the criminal case. This is discussed more in detail below.
2. Running Away Won’t Save You
Insurance fraud investigations take a long time. In some cases, the long periods between contact from the insurance company can lull people into a false sense of security. Many individuals believe that if the insurance company has not reached out for several months the matter must have resolved itself and gone away. This is almost never the case. The insurance company will never just “go away” when it comes to potentially fraudulent behaviour. While they may not contact you for several months at a time, this does not mean they are not still investigating.
Similarly, running away from the insurance company will not stop an investigation. Some individuals believe that if they leave their job the insurance company will not be able to find them or won’t bother going after them. This is untrue. It is not relevant whether you are still working for that employer, the insurance company will still attempt to collect on their losses.
Furthermore, for professionals such as nurses, doctors and teachers who are regulated by a College, being accused of defrauding your employee benefit plan may also trigger an investigation from the appropriate College. This, in turn, can impact an individual’s ability to practice in their given profession. In situations where an employee refuses to participate in the investigation in any way, the insurer will proceed without evidence from the accused individual, deciding in their absence.
Understanding Workplace Investigations
3. You Could be Criminally Charged and/or Sued
A common misconception many people hold when dealing with an insurance fraud investigation is that the consequences will only impact their job. Many people believe the worst that can happen if they get caught defrauding their employee benefits is that they may be terminated. While it is likely that an individual caught defrauding their insurance benefits will be terminated, it is also possible for the individual to be criminally charged with fraud and/or be sued in civil court.
If an individual’s employer or the insurance benefit provider decide to report the alleged fraud to police, a benefit holder could be charged with either fraud under $5,000 or fraud over $5,000 depending on the value of the fraud. An individual who is convicted of either of these offences will have a criminal record which can have many negative implications on an individual’s life. Further, those who are convicted of fraud may face a period of incarceration.
Fraud Under $5,000
Where the Crown proceeds by summary conviction, an accused who is convicted will face a maximum of two years less a day in prison and/or up to a $5,000 fine. Where the Crown proceeds by indictment an accused will face a maximum of two years in prison upon conviction.
Fraud Over $5,000
Fraud over $5,000 is a straight indictable offence. Those who are convicted will face a maximum of fourteen years in prison.
It is also important to note that there is no limitation period on when an individual can be charged for fraud if the Crown elects to proceed by indictment. This means that an individual may be charged and convicted of a fraud offence years, or even decades after the offence is committed.
4. Forgoing Documents will make things Worse
In some situations, individuals may attempt to create receipts for services they did not receive or alter receipts for services they did receive. This is a big mistake. Not only will this not help your case, but it may lead to additional criminal charges being laid if law enforcement gets involved.
When receipts are provided to the insurance company in the course of a fraud investigation, they will be diligently verified with the service provider, confirming that the client attended the service provider on the date on the claim and paid the amount listed on the claim. If any of the details do not match, the insurer will deem the claim fraudulent.
Since insurers verify all receipts, it is very likely that an individual who submits fraudulent receipts will get caught. This may make the insurer more willing to contact law enforcement. If law enforcement is contacted as a result, the individual may face charges for fraud as well as charges for forgery and/or use, trafficking, or possession of a forged document
Law Newbie is a free AI research assistant that can help you safely answer questions about criminal law.




5. Anything you Say can and Will be Used Against You
It is important to be aware that anything you say to anyone from your employer or from the insurance companies is likely being recorded and may be used against you in the future. This includes any admissions and/or utterances. Insurance companies are private entities, meaning the Charter of Rights and Freedoms does not apply. This means individuals accused of defrauding their insurance benefit plan have fewer rights and protections during the insurance companies’ investigation than they would during a police investigation.
Anything you say to the insurance company could also be brought in as evidence against you should the insurance company or your employer take their allegations to the police. The admission of such evidence in a criminal or civil trial could lead to the individual being convicted or ordered to pay the money back plus interest and court costs.
Since the Charter does not apply and individuals have fewer rights, insurance companies can get away with a lot more during an investigation. As a result, it is important to protect your rights as soon as the insurance company has brought any discrepancies to your attention. As a general rule, apologizing and paying back the money will not stop the investigation and will not protect you from being arrested or sued.
6. If you Are a Regulated Professional Your License Could be Affected
For individuals who are regulated professionals such as accountants, nurses or teachers, an employee insurance benefit fraud investigation could also trigger an investigation from the respective regulatory body.
At the completion of the insurance companies’ investigation, if the professional is found to have committed insurance benefit fraud, the appropriate College may be notified by the individual’s employer. In other cases, the College may have self-reporting regulations, requiring the professional to report the fraudulent behaviour to their regulatory College on their own. If criminal charges are laid, this could complicate matters with a regulatory body even further.
Each regulatory body prosecutes professionals under their mandate in a different way. Professionals who are found to have committed a criminal offence could be found guilty of misconduct by the regulatory body. This could result in conditions being applied to the Member’s license or the Member’s license being revoked or suspended.
7. Your Immigration Status could be Impacted
Individuals who are not Canadian citizens may face additional consequences if they become involved in an insurance fraud investigation. If the individual is charged with a fraud offence as a result of the investigation, their immigration status may be impacted. Those are convicted of certain crimes may be deported from Canada as a result.
Fraud over $5,000 is a straight indicatable offence. Being convicted of this offence and sentenced to a period of incarceration may lead to deportation. If you have been accused of insurance benefit fraud and are not a Canadian citizen, it is important to contact counsel to determine how the investigation could impact your immigration status.
If your insurance company has brought discrepancies in your insurance claims to your attention, it is important to contact experienced legal counsel as soon as possible. If contained early on, it is possible to settle the matter without involving law enforcement. Donich Law has experience defending individuals accused of stealing from and defrauding their employers and regularly achieves favourable outcomes for our clients.
How Insurance Investigations Start
Is it Easy to be Accused of Benefits Fraud?
Being accused of committing insurance benefit fraud can be a stressful and unsettling experience. With advances in technology, many benefit users can now submit claims online without providing paper receipts up front. While online services make filing claims simple for users, they also make it possible for users to submit fraudulent claims and receive money that they are not entitled to. As a result, insurance companies have developed sophisticated techniques to screen claims and catch fraudsters.
In some cases, benefit users may be accused of committing benefit fraud even when they did not intentionally do so. For example, failure to accurately submit online claims could result in overpayment from the insurance company. This overpayment will be considered fraudulent.
Insurance benefit fraud investigations arise generally in one of four ways; the plan member is contacted directly by the insurance company, the plan member is contacted by their employer, the plan member is caught as part of a sting investigation, or the plan member is involved in a joint investigation involving both their employer and insurance benefit provider.
Plan Member Contacted by Insurance Company
With more and more online claims being accepted by insurance companies, insurance benefit fraud has become easier to commit. To combat this, insurance companies have developed sophisticated techniques to investigate potential fraud.
Insurance companies employ entire departments of employees dedicated to tracing and tracking down fraudsters. Fraud departments at insurance companies will work to verify claims submitted to ensure the claims were submitted accurately and that the benefit user was entitled to the benefits received. If the insurance company comes across a claim it cannot verify or a claim that is deemed fraudulent, it could trigger an audit, causing the insurance company to attempt to verify all claims submitted by the user.
The insurance company may contact the service provider to confirm services were rendered as claimed. If the service provider is unable to verify the claim, the insurance company will reach out to the benefit user to verify the claim. If the benefit user is unable to verify the claim, the claim will likely be deemed fraudulent.
If you have been contacted by your insurance benefit provider in reference to unverified claims, it is important to consult with legal counsel prior to communicating with the insurance company investigator. Any admissions made, or evidence provided could later be used against an accused in civil or criminal court.
Employer Ambush
In some cases, when insurance fraud allegations are leveled at an employee, the employer will become involved in the investigation. This is common where the fraud resulted in an employer loss rather than an insurance company loss. In these cases, it is common for the employer to call a meeting with the impugned employee in an attempt to solicit a confession.
In these scenarios, employees often feel compelled to participate in the employer investigation or risk employment consequences. However, in many cases the risk associated with cooperating with the investigation is greater than the risk of refusing. In almost all cases, if the employee has committed benefit fraud, they will be terminated regardless of whether or not they cooperate with the investigation. As a result, there is often no benefit to participating in any meetings with the employer. Any admissions made to one’s employer could later be used in court to gain a fraud conviction.
If you have been accused of employee insurance benefit fraud and have been asked to participate in a meeting to discuss the matter, it is important to consult with legal counsel prior.
Stings
Another common way individuals are caught committing employee benefit fraud is through sting investigations. Sting investigations may occur where a number of people are participating in an insurance fraud scheme. Such a scheme could involve several employees from the same organization all filing false claims for services from the same service provider. In these situations, the discovery of one fraudulent claim could lead to the discovery of many fraudulent claims from many different employees within one organization. Sting investigations often result in the termination of a large number of employees at one time.
Joint Investigations
In some cases, both the insurance company and the employer will investigate the potential benefit fraud in tandem. This may occur where both parties have experienced a loss as a result of the fraudulent behaviour. In a joint investigation the risk of the matter being reported to law enforcement increases since both the employer and the insurance company may report the allegations.